Understanding Osteoarthritis: Detailed Guide
Dr. Jane Doe
7 Sep 2024 • 8 min read
Introduction to Osteoarthritis
Osteoarthritis (OA) is the most common form of arthritis, affecting millions of people worldwide. It occurs when the protective cartilage that cushions the ends of the bones wears down over time, leading to pain, stiffness, and reduced joint mobility. Although osteoarthritis can damage any joint, it most commonly affects joints in the hands, knees, hips, and spine.
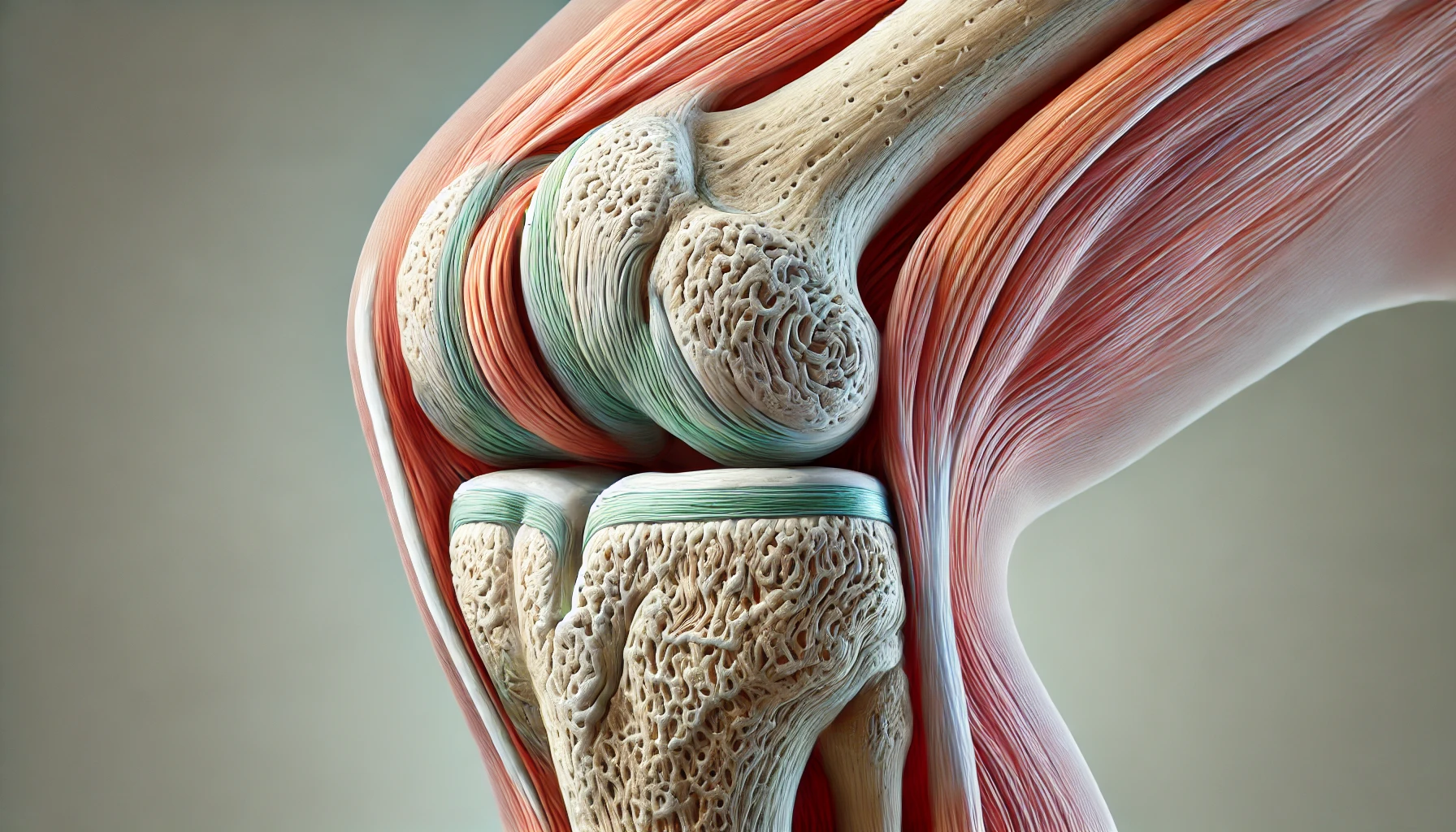
What is Osteoarthritis?
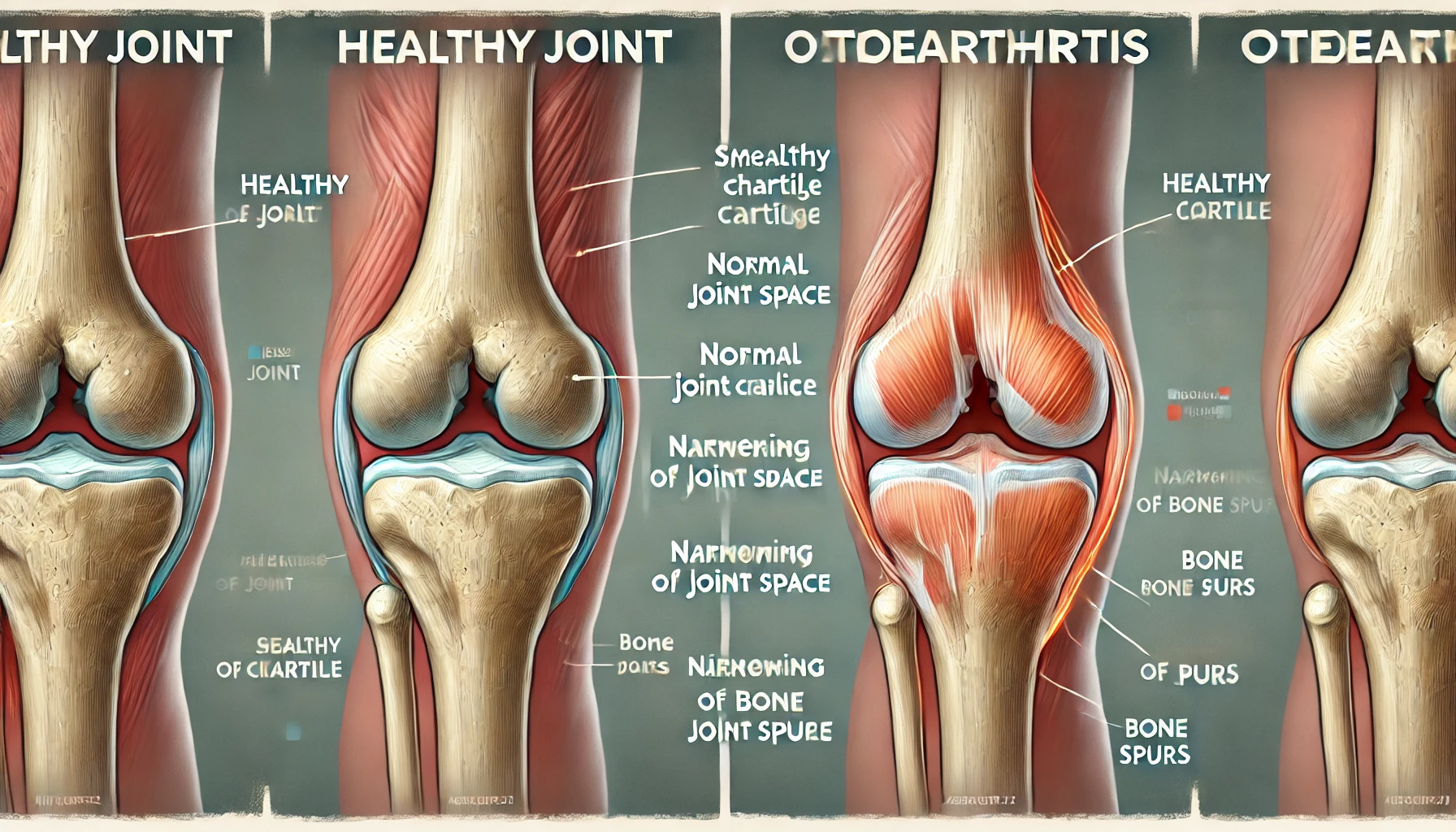
Osteoarthritis is a degenerative joint disease characterized by the breakdown of cartilage, the smooth, slippery tissue that covers the ends of bones in a joint. As the cartilage deteriorates, the underlying bone may thicken and develop bony growths called osteophytes. This process can lead to pain, swelling, and difficulty moving the joint.
Symptoms of Osteoarthritis
- Joint Pain: Pain during or after movement, often worsening with activity.
- Stiffness: Joint stiffness, especially after waking up or being inactive.
- Tenderness: The joint may feel tender when applying light pressure.
- Loss of Flexibility: Reduced range of motion in the affected joint.
- Grating Sensation: A feeling of grating or a 'crunching' sound when moving the joint.
- Swelling: Swelling around the joint due to inflammation.
- Bone Spurs: Extra bits of bone that form around the affected joint.

Causes and Risk Factors
Osteoarthritis occurs when the cartilage that cushions the ends of bones in the joints gradually deteriorates. Factors that contribute to the development of osteoarthritis include:
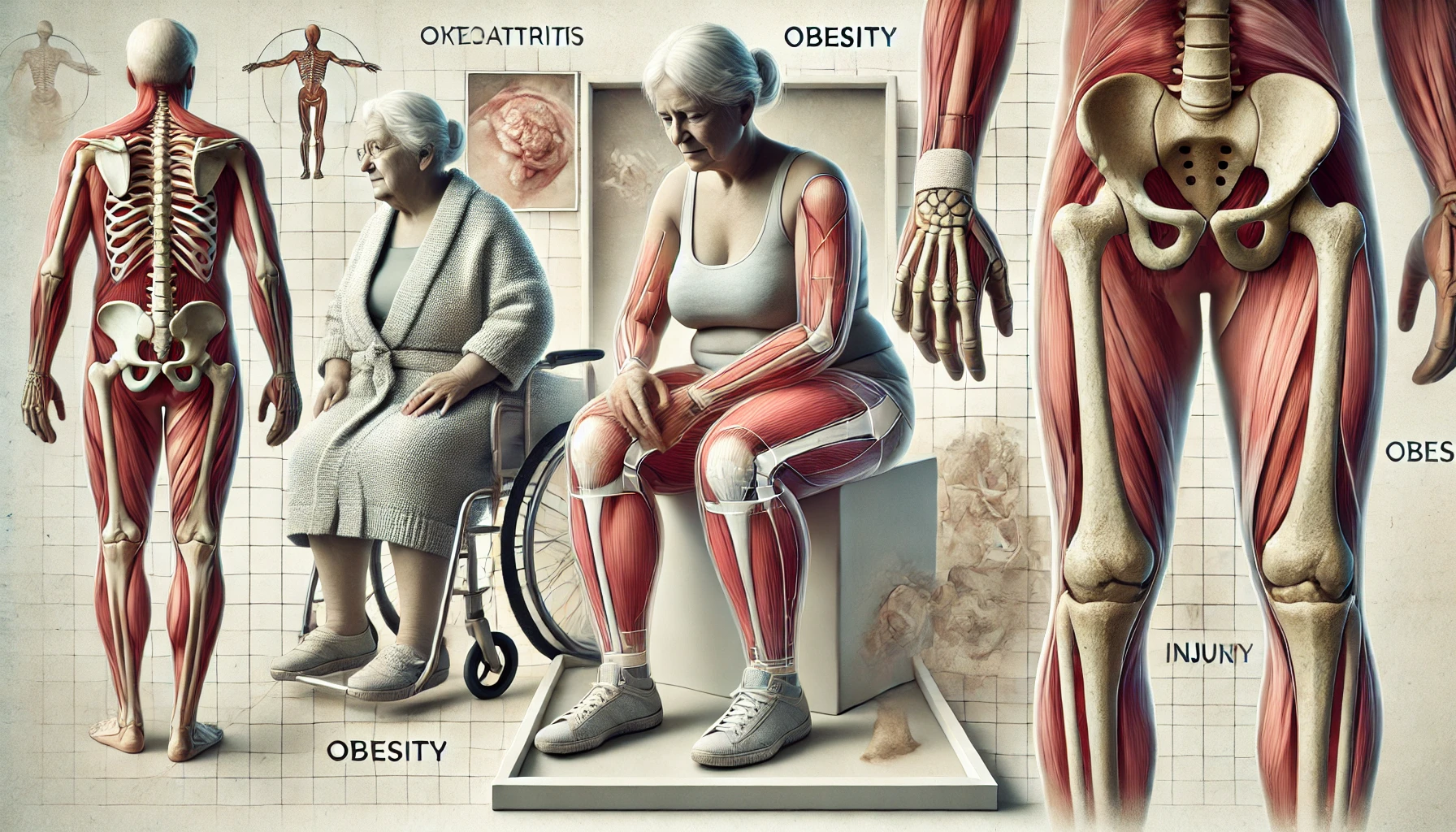
- Aging: The risk of osteoarthritis increases with age as the cartilage naturally wears down.
- Joint Injury: Previous joint injuries, such as those from sports or accidents, can increase the risk.
- Obesity: Excess body weight puts additional stress on weight-bearing joints, such as the knees and hips.
- Genetics: A family history of osteoarthritis can increase the likelihood of developing the condition.
- Overuse of Joints: Repetitive movements and overuse of certain joints can lead to osteoarthritis.
- Bone Deformities: Some people are born with malformed joints or defective cartilage, increasing the risk of osteoarthritis.
Diagnosing Osteoarthritis
Diagnosing osteoarthritis typically involves a combination of physical examinations, medical history, and imaging tests:
- Physical Examination: The doctor will examine the affected joints for signs of swelling, tenderness, and limited range of motion.
- Imaging Tests: X-rays can show bone spurs and cartilage loss. MRI provides detailed images of bones, cartilage, and other structures to help diagnose osteoarthritis, especially in its early stages.
- Lab Tests: Joint fluid analysis can check for inflammation or infection, and blood tests help rule out other forms of arthritis.

Treatment Options
There is no cure for osteoarthritis, but treatment focuses on managing symptoms and improving joint function. Common treatment options include:
- Pain Relievers: Acetaminophen or NSAIDs to relieve pain and reduce inflammation.
- Corticosteroid Injections: Help reduce inflammation and provide temporary pain relief.
- Hyaluronic Acid Injections: Lubricate the joint and act as a shock absorber.

Lifestyle Changes and Home Remedies
- Exercise Regularly: Engage in low-impact exercises such as walking, swimming, or cycling to maintain joint flexibility and strength.
- Apply Hot and Cold Compresses: Heat can relieve stiffness, while cold can reduce pain and swelling.
- Maintain a Healthy Diet: Focus on a balanced diet rich in fruits, vegetables, and omega-3 fatty acids to help reduce inflammation.
- Use Assistive Devices: Use braces or shoe inserts to reduce stress on affected joints.
- Practice Good Posture: Avoid putting unnecessary stress on your joints by practicing proper posture and body mechanics.

Complications of Osteoarthritis
Osteoarthritis can lead to several complications, including:
- Chronic Pain: Persistent pain can affect daily activities and quality of life.
- Decreased Mobility: Joint stiffness and pain can lead to difficulty moving and performing everyday tasks.
- Sleep Disturbances: Pain and discomfort can interfere with sleep.
- Depression and Anxiety: The physical limitations of osteoarthritis can lead to emotional challenges.
- Joint Deformity: In severe cases, the joint may lose its normal shape, leading to deformity.

Preventing Osteoarthritis
While osteoarthritis cannot always be prevented, certain strategies can reduce the risk:
- Maintain a Healthy Weight: Keeping weight within a healthy range reduces stress on joints.
- Stay Active: Regular physical activity strengthens muscles and maintains joint flexibility.
- Avoid Joint Injuries: Protect your joints during activities and avoid repetitive stress.
- Practice Good Posture: Proper posture and body mechanics reduce the risk of joint strain.
- Eat a Healthy Diet: A balanced diet supports overall health and reduces inflammation.

Advances in Osteoarthritis Research and Treatment
Recent advancements in osteoarthritis research have led to new treatment options and improved management strategies. These include:
- Regenerative Medicine: Research into stem cell therapy and platelet-rich plasma (PRP) injections to repair damaged cartilage.
- New Medications: Development of drugs that target inflammation and pain specifically associated with osteoarthritis.
- Minimally Invasive Surgeries: Techniques that reduce recovery time and improve outcomes for joint replacement or repair.
- Wearable Technology: Devices that monitor joint health and provide feedback to help manage symptoms.

Conclusion
Osteoarthritis is a common but manageable condition that requires a comprehensive approach to treatment and lifestyle changes. By understanding the causes, symptoms, and available treatment options, individuals with osteoarthritis can take steps to improve their quality of life and reduce the impact of the disease on their daily activities. Remember to consult with healthcare professionals for personalized advice and support.

Dr. Jane Doe
7 Sep 2024 • 8 min read